Pharmacology of Opioid Analgesia
Opioids are a class of powerful drugs commonly used for pain management due to their ability to provide effective analgesia. They work by binding to opioid receptors in the CNS, where they reduce the transmission of pain signaling. This binding also triggers the release of several neurotransmitters that work to dampen pain perception and produce feelings of euphoria and relaxation. As such, while opioids can be very effective for analgesia, their use comes with major risks, including addiction, due to their overt impact on the brain’s reward system. Understanding the pharmacology of opioid analgesia, including their mechanisms of action, uses, and potential adverse effects, is critical for their safe and appropriate use in clinical environments.
There are many opioid receptors within the CNS, as well as throughout peripheral tissues. Among the three main classes of opioid receptors, the most prevalent receptor is the mu (µ) receptor, which can be found in the brainstem and medial thalamus. This receptor group is responsible for supraspinal analgesia, respiratory depression, euphoria, sedation, decreased gastrointestinal motility, and physical dependence. The Mu1 subtype is more heavily associated with analgesia, euphoria, and relaxation, while the Mu2 subtype is linked to respiratory depression, prolactin release, dependence, anorexia, and sedation. Kappa (κ) receptors can be found in the limbic and other diencephalic areas, the brainstem, and spinal cord. This group is responsible for spinal analgesia, sedation, dyspnea, dependence, and dysphoria. Finally, delta (δ) receptors are rarer and not as well studied. They are thought to control psychomimetic and dysphoric responses.1
Typically, these receptors are stimulated by endogenous pro-hormone precursors which are produced in response to noxious stimulation. When an opioid receptor agonist binds to a G-protein-coupled receptor, the α subunit of the G-protein exchanges its bound guanosine diphosphate (GDP) molecule with intracellular guanosine triphosphate (GTP). As a result, the α-GTP and βγ complexes become free to interact with their target proteins. Inhibition of adenylyl cyclase causes a reduction in intracellular cyclic adenosine monophosphate (cAMP).2 The α-GTP and βγ complexes also interact with ion channels to activate potassium conductance and inhibit calcium conductance, leading to hyperpolarization of the cell and decreased neurotransmitter release.3
The pharmacology of opioid analgesia centers largely around activation of mu receptors. In these cases, mu agonists indirectly stimulate descending inhibitory pathways to activate associated neurons. Increased neuronal traffic in the nucleus raphe magnus (NRM) increases stimulation of neurons connected to the substantia gelatinosa of the spinal dorsal horn. Ultimately, this cascade results in reduced nociceptive transmission from the peripheral tissues to the thalamus.2
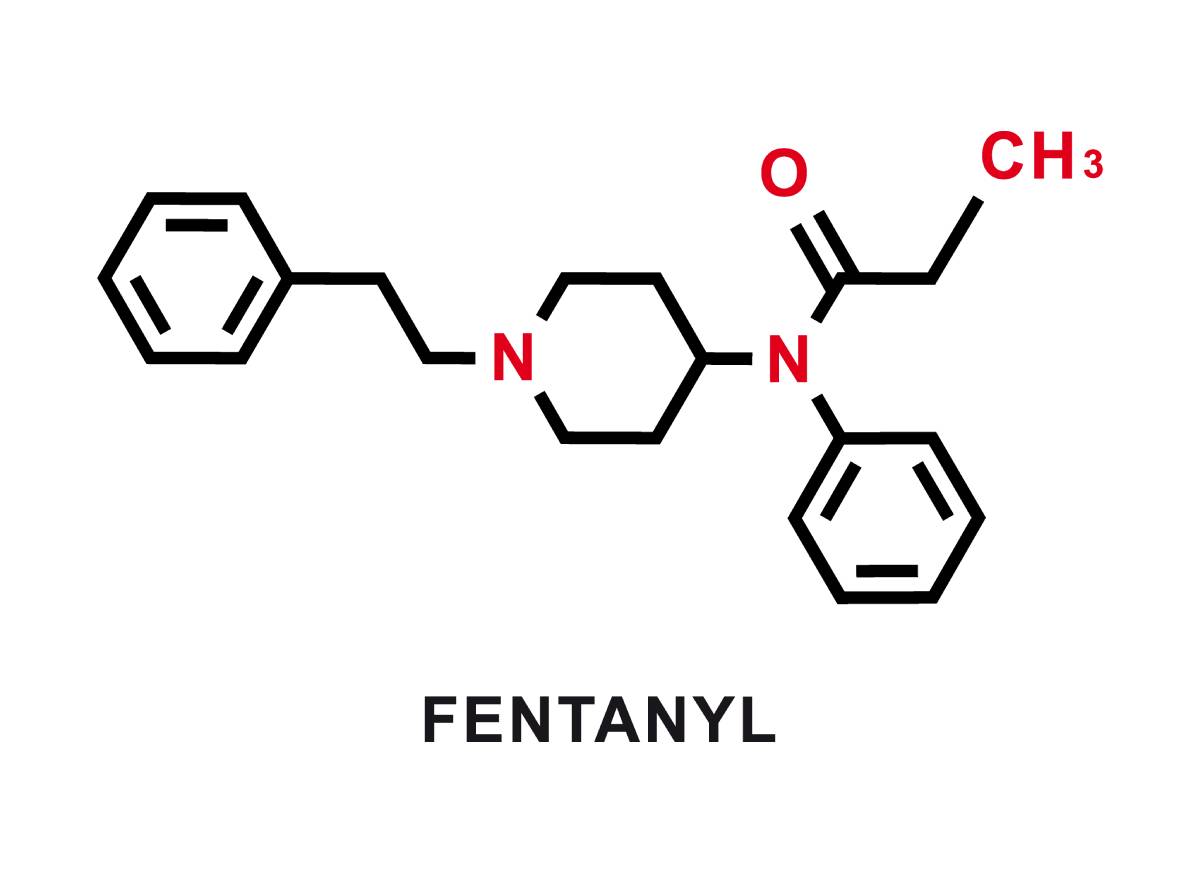
Morphine, an opioid with widespread use in medicine, acts primarily on the mu receptor and partially on the kappa and delta receptors. Other commonly used opioids include alfentanil, fentanyl and remifentanil, which also act on mu receptors. Alfentanil and fentanyl are highly lipid soluble and have a far more rapid onset of action than morphine. However, their high lipid solubility can result in sequestration of the drug to fat stores, leading to extended recovery times where the drug must be extracted from fatty tissues before renal excretion.4 On the other hand, remifentanil has a novel mechanism of metabolism where it is metabolized extrahepatically by non-specific esterases in blood and tissue. Although remifentanil is significantly more lipid soluble than morphine, its unique pharmacology makes it a preferred opioid analgesia agent in many situations where rapid drug clearance is ideal.2
Opioids are highly effective in pain management, primarily through their action on the mu, kappa, and delta receptors in the CNS. However, their use comes with significant risks, including the possibility of addiction, respiratory depression, and physical dependence. A thorough understanding of opioid pharmacology, including receptor interactions and individual drug characteristics, is essential for ensuring their safe and effective use for analgesia.
References
- Trescot, A. M., Datta, S., Lee, M., and Hansen, H. (2008). Opioid Pharmacology. Pain physician, 11(2S), S133-S153.
- Pathan, H., and Williams, J., “Basic Opioid Pharmacology: An Update.” British Journal of Pain, 6(1), 2012, 11–16. https://doi.org/10.1177/2049463712438493
- Corbett, A.D., et. al., “75 Years of Opioid Research: The Exciting but Vain Quest for the Holy Grail.” British Journal of Pharmacology, 147(S1), 2006. https://doi.org/10.1038/sj.bjp.0706435
- Nielsen, C.K., et. al. “Oxycodone and Morphine Have Distinctly Different Pharmacological Profiles: Radioligand Binding and Behavioural Studies in Two Rat Models of Neuropathic Pain.” Pain, 132(3), 2007, 289–300. https://doi.org/10.1016/j.pain.2007.03.022
